Many would be forgiven for assuming that podiatry and nephrology are not closely related. After all, geographically, the feet are a long way from the kidneys. However Podiatrists play an important role in the early detection of kidney problems, assist in the management of some symptoms of kidney disease, and provide ongoing care for those with acute lower limb concerns stemming from systemic disease.
One of the primary roles of a Podiatrist relates to the monitoring and assessment of oedema in the lower limb. Oedema is a sign of higher-level health problems, which need to be addressed. However, oedema can also cause:
- Pain due to swelling
- Difficulty walking
- Stretched and stressed skin which is at risk of breakdown
- Increased risk of infection in the swollen area, which is commonly known as cellulitis
- Scarring between layers of tissues
- Decreased circulation
- Decreased elasticity of blood vessels, muscles, and other soft tissues
- Increased risk of thrombosis due to decreased circulation
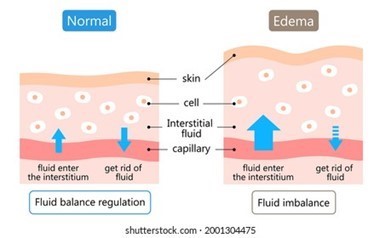
Glomerular diseases (which reduce the kidneys’ ability to maintain a balance of certain substances in the bloodstream) can both cause systemic health problems and be affected by systemic disease. Kidneys primarily function to filter the blood and clear waste and toxins. Nephrotic syndrome occurs when glomerular capillary walls do not work properly, and more plasma proteins are able to pass through. As a result, we see higher than recommended protein loss through urine. This sees a depletion of serum albumin in the blood and a loss of Colloid Osmotic Pressure (COP), which in turn leads to an increase fluid in interstitial tissues: oedema.
The primary objective of health professionals when this occurs is to address the cause of the nephrotic syndrome. However, it is also important to manage the side effects of oedema. This is where podiatrists are often brought in to perform vascular assessments of the lower limb.
This assessment involves checking pulses, through both palpation and using a doppler to listen to the arterial and venous flow, testing venous function, and performing ABI assessments. Podiatrists will also examine the skin integrity, joint range of motion, sensation, and importantly footwear. After this, the client may be referred to a vascular specialist if peripheral vascular disease is also suspected; but the podiatrist may also recommend compression garments for the management of fluid volumes and ongoing protection of skin integrity.
As nephrotic syndrome and the subsequent oedema directly affects COP, it also can affect oxygenation of peripheral tissues. This can put the client at risk of wounds, but also lead to increased tissue stress and subsequent hyperkeratotic skin lesions. Podiatrists can direct wound management, but also assist by debriding and making recommendations for the management of the skin lesion.


If a patient’s feet are swollen there are also often concerns regarding footwear. Podiatrists are able to assess the suitability of existing footwear, make modifications where needed, or recommend alternative footwear options to provide comfort to the client and also prevent pressure injuries.
Our Plena podiatry team assist all of these processes and can perform most assessments on the spot. However, some prior arrangements are required for doppler assessments.
Click here to find out more about our podiatry services or to enquire.



